Background & Purpose
Federal COBRA continuation rights are triggered when there is a loss of coverage caused by one of the following:
- voluntary or involuntary termination of employment other than by reason of gross misconduct;
- reduction of hours of the covered employee's employment;
- divorce or legal separation of the covered employee from the employee's spouse;
- death of the covered employee;
- a dependent child ceases to be a dependent under the generally applicable requirements of the plan;
- a covered employee becomes entitled to benefits under Medicare; and
- an employer's bankruptcy, but only with respect to health coverage for retirees and their families.
COBRA continuation rights for the employee, spouse or dependents enrolled in the plan are for up to 18 months for the following:
- covered employee's termination of employment (other than for gross misconduct); and
- covered employee's reduction of hours.
COBRA continuation rights for the spouse or dependents enrolled in the plan are for up to 36 months for the following:
- death of the covered employee;
- divorce or separation of the covered employee from his or her spouse;
- the covered employee's becoming entitled to Medicare benefits; and
- a dependent child's ceasing to be a dependent.
COBRA continuations for a retiree, spouse or dependents enrolled in retiree coverage are for the life of the retiree upon the employer’s bankruptcy. If the spouse or dependents survive the retiree, they are entitled to coverage for up to 36 months following the retiree’s death.
The maximum coverage period can run from the qualifying event date. Or, if the loss of coverage occurs later (e.g., end of the month in which eligibility is lost), the employer can choose instead to have it run from the actual loss of coverage. The employer should choose one method or the other and apply it consistently.
While the maximum coverage period is generally, 18, 29 or 36 months, as described above, there are several ways that the maximum period of COBRA coverage can be extended. These extensions are described below.
Disability Extension
The purpose of this extension is to allow for disabled individuals to be able to receive COBRA coverage until they may be eligible for Medicare. To be eligible for Medicare, an individual must be entitled to Social Security disability insurance for at least 24 months, and there is a 5-month waiting period before monthly disability benefits begin. This extension can then extend the maximum COBRA coverage period to 29 months.
For this extension to apply, the following requirements must be met.
- The qualifying event giving rise to the right to COBRA coverage must be either a termination of employment or a reduction of hours for the covered employee.
- A qualified beneficiary must be determined to be disabled by the Social Security Administration (SSA) during the first 60 days of COBRA coverage. There should be a letter from the SSA setting forth this determination.
- The first 60 days of COBRA coverage is measured from the date of the qualifying event unless the extended notice rule applies, in which case the date of the loss of coverage is used.
- For COBRA coverage for a child born to or adopted by the covered employee while on COBRA coverage, the first 60 days of COBRA coverage is measured from the date of birth or adoption.
- Both the IRS and the DOL have recognized that a Social Security determination of disability may be issued before a qualifying event and still meet the requirement that the qualified beneficiary be determined to be disabled within the first 60 days of COBRA coverage.
- A qualified beneficiary must notify the plan administrator of the determination of disability before the end of the 18-month period following the qualifying event and within 60 days of the latest of the:
- Date of the determination of disability;
- Date of the qualifying event;
- Date that the disabled qualifying beneficiary lost coverage; or
- Date that the disabled qualifying beneficiary is first informed of the responsibility to notify the plan administrator of the disability determination and the plan’s procedures on how to get notice to the plan administrator.
Once a determination of disability is made and the plan administrator has been notified of such determination, the 29-month extension then applies to all qualified beneficiaries in connection with a qualifying event – not just to the qualified beneficiary determined to have a disability. In fact, the qualified beneficiary deemed to be disabled does not even have to elect COBRA coverage for the related qualified beneficiaries to receive the 29-month period of coverage. This also means that if the disabled qualified beneficiary does elect COBRA, but drops or loses COBRA coverage early, the remaining qualified beneficiaries on COBRA coverage may continue with the extension.
However, if the disabled qualified beneficiary is determined to no longer be disabled by the Social Security Administration, all qualified beneficiaries will lose the 29-month extension. This means that upon a determination of no longer disabled during the extension of coverage (beyond the original 18 months of COBRA coverage), COBRA coverage would then be terminated for all related qualified beneficiaries.
For any extension beyond the original 18-month maximum period of coverage that is solely due to this disability extension, the plan may charge the disabled qualified beneficiary 150% of the applicable premium (instead of the standard limit of 102%).
Multiple Qualifying Events
Also known as a second qualifying event, this extension will apply if, during their 18-month (or 29-month if the disability extension applies) period of COBRA coverage as triggered by a first qualifying event, a qualified beneficiary experiences another qualifying event that would trigger a 36-month maximum period of COBRA coverage. This rule cannot extend the period of COBRA coverage for a covered employee. The only qualified beneficiaries whose COBRA coverage may be extended under this rule are the covered employee’s dependents and spouse that elected COBRA coverage upon the first qualifying event. This extension rule will apply to a spouse and dependents that elected COBRA regardless of whether the covered employee elected COBRA coverage upon the first qualifying event.
For this extension to apply, the following requirements must be met.
- The original qualifying event giving rise to the right to COBRA coverage must be a termination of employment or reduction of hours.
- The second qualifying event must be one that gives rise to a maximum period of COBRA coverage of 36 months, including:
- Death of the covered employee;
- Divorce or legal separation from the covered employee; and
- Dependent ceases to be a dependent.
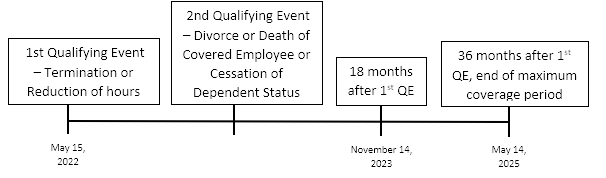
Importantly, however, the 36-month period of COBRA coverage will run from the start date of the original 18-month (or 29-month) maximum coverage period, rather than from the date of the second qualifying event. The below timelines illustrate an example of an 18-month first qualifying event followed by a second qualifying event. Also note that these timelines do not demonstrate the extended notice rule. If the extended notice rule were implemented, then the coverage periods would run from the date that coverage is lost, not the date of the qualifying event.
Medicare Entitlement Prior to Employee’s Termination of Employment or Reduction in Hours
Like the multiple qualifying event extension, this extension will extend COBRA coverage only for the covered employee’s spouse and dependents. A covered employee’s COBRA coverage cannot be extended under this rule. In this extension, the covered employee’s Medicare entitlement must occur before the qualifying event for the spouse and dependents. If the qualifying event occurs on the same day as, or after, the covered employee’s Medicare entitlement, this extension would not apply.
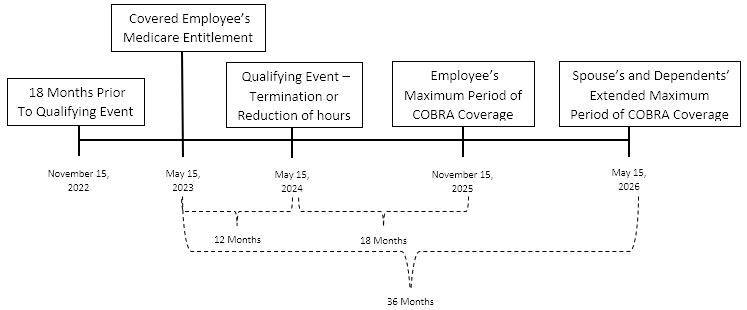
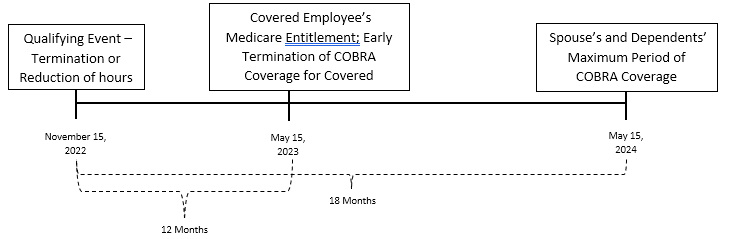
If the employee’s termination of employment or reduction in hours occurs within 18 months after the employee’s entitlement to Medicare (actual enrollment in Medicare, not just eligibility), the spouse and dependents who elect COBRA have continuation rights for the longer of:
- 18 months from the qualifying event (or loss of coverage); or
- The remainder of 36 months from the employee’s Medicare entitlement.
The below timelines illustrate examples of how the order of events would affect a spouse and any dependent’s maximum period of COBRA coverage.
Pre-Termination/Pre-Reduction Medicare Entitlement Extension Does Apply
Pre-Termination/Pre-Reduction Medicare Entitlement Extension Does Not Apply
While every effort has been taken in compiling this information to ensure that its contents are totally accurate, neither the publisher nor the author can accept liability for any inaccuracies or changed circumstances of any information herein or for the consequences of any reliance placed upon it. This publication is distributed on the understanding that the publisher is not engaged in rendering legal, accounting or other professional advice or services. Readers should always seek professional advice before entering into any commitments.

